Have you ever felt like the classic, hyperactive image of ADHD doesn't quite capture your own experience? If you’ve wondered about the difference between ADHD and ADD, you’ve landed in the right place.
Here’s the simple truth: ADD is an outdated term.
What was once called ADD is now officially known as Attention-Deficit/Hyperactivity Disorder (ADHD), Predominantly Inattentive Presentation. This distinction is more than just words—it’s about finally having a language that validates the quiet, internal struggles so many people face.
Understanding Today's ADHD Diagnosis
If you were diagnosed with ADD years ago, that diagnosis is an absolutely valid part of your story. The change simply means the medical community now uses ADHD as a single umbrella term to describe the condition more accurately and inclusively.
This shift reflects a much deeper scientific understanding of how ADHD shows up in different people. The term ADD first appeared in the 1980s, but by 1987, the official name became the broader ADHD. This was a crucial change, recognizing that inattention and hyperactivity were part of the same condition, not separate ones.
This updated framework helps bust common ADHD myths and misconceptions, especially the idea that you have to be bouncing off the walls to have ADHD.
💡 Key Takeaway: You don’t have “just” an attention problem or “just” a hyperactivity problem. ADHD is a complex condition affecting the brain’s self-management system, and it can look and feel different for everyone.
From Old Terms to New Understanding
For example, what was once known as ADD is now referred to as ADHD, Predominantly Inattentive Presentation. This means your experience may center on challenges with focus, organization, and follow-through, without significant outward hyperactivity.
Similarly, ADD with Hyperactivity is now ADHD, Combined or Hyperactive/Impulsive Presentation. In this case, your experience may include both inattentive traits and visible signs of hyperactivity or impulsivity.
Ultimately, this modern understanding allows for more nuanced and accurate diagnoses, ensuring people receive support that truly fits their experience, whether it's visibly hyperactive or quietly inattentive.
Have you noticed how these older terms might have limited how people saw their own struggles?
The Journey from ADD to a Broader ADHD Diagnosis
If you still find yourself using the term ADD, you're not alone. It feels familiar for a reason—for many years, it was the official term clinicians used. The shift from ADD to ADHD wasn't just a simple name change; it marked a huge step forward in how we understand this neurotype.
This evolution is tracked in the Diagnostic and Statistical Manual of Mental Disorders (DSM), the guidebook for mental health diagnoses. Back in 1980, the DSM-III introduced Attention Deficit Disorder (ADD). At that point, you could be diagnosed with ADD with or without hyperactivity, as they were seen as separate features.
This infographic lays out how the official language has changed over the decades, reflecting a deeper scientific consensus.
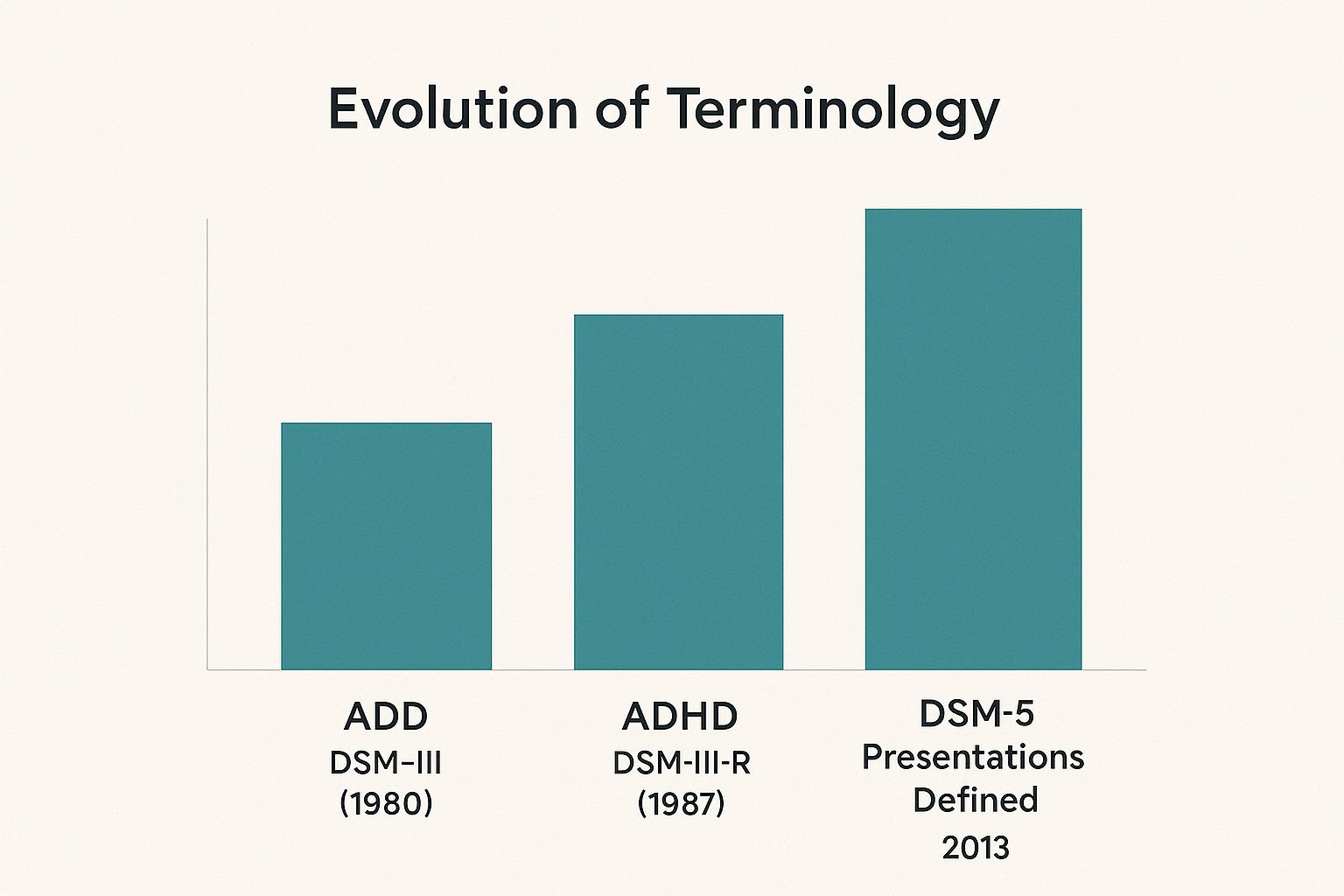
The big moment came in 1987 when the DSM-III-R officially combined everything under the single diagnosis of ADHD.
A More Inclusive Understanding
By the late '80s, the thinking had shifted. Researchers began to see that inattention and hyperactivity weren't two separate conditions but different expressions of the same underlying neurodevelopmental differences. This insight led to ADHD becoming the single, umbrella term.
🔬 Scientific Takeaway: The move to "ADHD" was a major confirmation that hyperactivity isn't a mandatory symptom. Instead, it's one of several potential traits—along with inattention and impulsivity—that all exist on a spectrum.
This was a game-changer, especially for recognizing how ADHD shows up in girls and women, who are far more likely to have the quieter, inattentive presentation that the old models often missed.
Today, the most current manual, the DSM-5, doesn't use the term ADD at all. Instead, it specifies one of three "presentations" of ADHD. This refined approach helps ensure everyone’s experience gets validated.
Exploring the Three Faces of ADHD

Now that we're clear ADHD is the official term, let's explore what it actually looks like. It’s not a one-size-fits-all diagnosis; think of it more like a spectrum of experiences.
To capture this, the DSM-5 outlines three distinct "presentations." Finding where you fit can feel like someone finally handed you the right map for your brain. It explains why one person with ADHD is full of restless energy while another feels like they're walking through a constant mental fog.
Predominantly Inattentive Presentation
This is what people used to call ADD. If you recognize yourself here, you're likely familiar with the quiet, internal battle of feeling spacey, disorganized, or constantly forgetting things. It isn't because you don't care; it's a genuine challenge with executive functions.
✅ Common experiences you might recognize:
- Struggling to finish projects, even stuff you genuinely enjoy.
- Losing your keys, phone, or wallet on a near-daily basis.
- Getting easily sidetracked by your own thoughts.
- Finding it hard to follow multi-step instructions.
Because these symptoms are less outwardly disruptive, they often fly under the radar, especially in girls and adults.
Predominantly Hyperactive-Impulsive Presentation
This is the classic picture most people have in their heads when they hear "ADHD." It can feel like you’re powered by an internal motor that won’t quit. The struggle isn't just about sitting still; it's a relentless need for movement and stimulation.
✅ Common experiences you might recognize:
- Constantly fidgeting, tapping your feet, or squirming.
- Feeling restless most of the time, like you always need to be doing something.
- A tendency to interrupt people or blurt out answers.
- Finding it almost impossible to wait your turn.
Combined Presentation
What if your brain feels like it's both racing a million miles an hour and drifting off into space at the same time? Welcome to the Combined Presentation. This is diagnosed when you meet the criteria for both inattentive and hyperactive-impulsive symptoms. It's the most common presentation in adults.
💡 A Note of Validation: It is completely normal to have a mix of symptoms. You might feel restless in a meeting but totally zoned out when trying to do chores. This doesn't mean you're inconsistent; it means your ADHD is dynamic.
Recognizing the Three Faces of ADHD
Here's a quick look at how the three official presentations of ADHD compare:
ADHD Presentation: Predominantly Inattentive
- Common Experiences You Might Recognize: "I'm always losing things." "People think I'm not listening, but my brain just wanders." "I can't seem to finish anything I start."
- Key Diagnostic Focus: A consistent pattern of at least 6 inattentive symptoms (or 5 for adults 17+).
ADHD Presentation: Predominantly Hyperactive-Impulsive
- Common Experiences You Might Recognize: "I feel like I'm driven by a motor." "I talk too much and interrupt people without meaning to." "Sitting still is torture."
- Key Diagnostic Focus: A consistent pattern of at least 6 hyperactive-impulsive symptoms (or 5 for adults 17+).
ADHD Presentation: Combined
- Common Experiences You Might Recognize: "My mind is both racing and foggy." "I'm restless, but I also lose track of conversations easily."
- Key Diagnostic Focus: Meets the criteria for both inattentive and hyperactive-impulsive presentations.
Understanding these nuances is an important first step toward self-compassion. When you can identify your specific patterns, you can start finding strategies that actually align with your brain.
Want to explore this more? Our full guide on ADHD subtypes and symptom presentations is a great next step.
Why the Inattentive Experience Is Often Missed
Have you ever felt like your struggles were invisible just because you weren’t “bouncing off the walls”? If so, you’ve stumbled upon a core reason why inattentive ADHD is so deeply misunderstood. For decades, the public image of ADHD has been a young, hyperactive boy, creating a massive blind spot in diagnostics.
This stereotype has had profound consequences, especially for girls, women, and adults. Because inattentive symptoms are mostly internal, they don't cause the same outward disruption as hyperactivity. Instead of interrupting the teacher, you might have been the kid quietly daydreaming by the window.

The Quiet Struggle of Internalized Symptoms
Society often mistakes quiet inattention for personality flaws. You may have been labeled “lazy,” “a daydreamer,” or “unmotivated,” when in reality, your brain was working overtime just to keep up.
These internalized experiences are just as real—and just as challenging—as external hyperactivity. You might recognize yourself in these patterns:
- Mental exhaustion: The constant effort to focus and organize your thoughts can be incredibly draining.
- Trouble with follow-through: Starting projects with tons of enthusiasm only to lose steam is a classic pattern.
- Feeling overwhelmed: Simple, multi-step tasks can sometimes feel like climbing a mountain.
- Emotional sensitivity: Many people with inattentive ADHD also grapple with rejection sensitivity and emotional regulation.
💡 A Moment of Validation: Your struggles are not a character flaw. The difficulty you have with focus, organization, and finishing tasks is a reflection of how your brain is wired—not a measure of your effort or worth.
Because these challenges aren't as obvious, many people with inattentive ADHD go undiagnosed for years. They develop complex coping mechanisms to mask their difficulties, which only adds to the feeling of being an imposter. For a deeper look at this, you can learn more about inattentive-type ADHD.
Recognizing that your quiet struggle has a name is the first, most powerful step toward getting the right support and building self-compassion.
How Diagnosis and Treatment Honor Your Unique Brain
Understanding your ADHD presentation is more than just an academic exercise—it’s the first step toward getting help that actually works for your brain. A thoughtful diagnosis goes way beyond a simple checklist.
A good clinician will dig into your specific mix of symptoms, life experiences, and personal struggles to pinpoint your exact ADHD presentation. This detail is the foundation for building a support plan that feels made for you.
Tailoring Support to Your Needs
When it comes to managing ADHD, there is no one-size-fits-all solution. Once your presentation is clear, support can be shaped to tackle your biggest challenges while playing to your strengths. This isn't about "fixing" you; it's about getting the right tools for your brain's unique wiring.
Personalized support might look like this:
- Medication: Some medications are better at boosting focus (a common need for inattentive types), while others are more effective for managing impulsivity.
- Therapy: Cognitive Behavioral Therapy (CBT) can be a game-changer for building practical skills, like creating systems to stay organized or learning to regulate intense emotions.
- Coaching: An ADHD coach can help you identify your strengths and develop real-world strategies for navigating work, relationships, and daily life.
Getting the right support is critical. Unfortunately, many people fall through the cracks. Between 2020 and 2022, while 11.3% of kids aged 5–17 in the U.S. had an ADHD diagnosis, about 30% received no specific medication or behavioral therapy in 2022. This gap shows why a personalized approach is so important. You can find more details in recent health data reports.
💡 The Empowering Message: A precise diagnosis isn't a label. It's a roadmap. It validates your struggles and unlocks personalized strategies that empower you to thrive.
Common Questions About ADHD and ADD
Even after getting the facts straight, it's normal to have lingering questions. The shift in terminology can be confusing, and everyone's experience is a little different.
Let's clear up some of the most common questions with empathetic answers grounded in today's understanding.
Can I still use the term ADD to describe myself?
Absolutely. If you were diagnosed with ADD years ago, that label is a real part of your story and how you came to understand your brain. Many people still prefer it because it feels more accurate to their experience, especially if hyperactivity isn't a daily struggle.
While a clinician today will use the official term “ADHD, Predominantly Inattentive Presentation,” the language you use for yourself is your call. What matters most is that it feels true to you.
Is one type of ADHD more severe than another?
Not really. Severity isn’t about which type you have—it’s about the impact your symptoms have on your life. A diagnosis is a tool for understanding, not for ranking your challenges against someone else's.
For instance, someone with what might seem like "mild" hyperactivity could be thriving, while a person with "severe" inattentive symptoms might find it incredibly difficult to keep up with their job and well-being. It’s all completely individual.
💡 It's All Relative: There’s no "best" or "worst" kind of ADHD. The only thing that matters is how your specific symptoms affect your ability to function and feel good in your own life.
Do ADHD presentations change over time?
Yes, and this is a really important point. Your ADHD isn't set in stone; it's common for your primary symptoms to shift as you go through different life stages.
A child’s very obvious hyperactivity might morph into a quieter, internal feeling of restlessness in adulthood. In the same way, the increasing demands of adult life—juggling a career, home, and finances—can make once-manageable inattentive symptoms suddenly feel overwhelming.
How does ADHD present differently in women?
This is a critical question. For decades, ADHD in women has been massively underdiagnosed, largely because it doesn't fit the stereotypical image of a hyperactive boy. For many women, the experience is much more internalized.
Instead of outward hyperactivity, it often looks more like this:
- Chronic self-doubt and feeling like an imposter.
- Feeling constantly overwhelmed by everyday tasks.
- Struggling with intense emotions and rejection sensitivity.
- Being labeled "spacey," "a daydreamer," or "ditzy."
Because this internal struggle is so easy for others to miss, many women don't get a diagnosis until they're well into adulthood, often after seeking help for related issues like anxiety or depression.
Knowing these patterns is the first step toward advocating for yourself. Have you noticed this pattern in your own life?